🚰 FIRST CATHETER = FOLEY CATHETER (Not Central Line!)
🔑 Clinical Decision Point
If NO EKG changes AND able to establish urine output → May avoid hemodialysis
Therefore: Foley catheter is the FIRST catheter to place in hyperkalemia, not a central line for dialysis access.
✅ Foley First When:
- No EKG changes present
- Hyperkalemia unexplained
- Clinical suspicion of obstruction
- Trying to avoid dialysis
- ANY bladder scan >300mL
⚡ Central Line When:
- EKG changes present
- K+ >7.5 mEq/L
- Symptomatic hyperkalemia
- Failed medical management
- Anuric or dialysis-dependent
🚨 Emergency Protocol: STABILIZE → FOLEY → SHIFT → REMOVE
• Onset: 1-3 minutes • Duration: 30-60 minutes • NO effect on K+ levels • ONLY if EKG changes present
• May reduce K+ 0.8-1.1 mEq/L in 4-6 hrs • Can prevent need for dialysis • Check bladder scan • Post-void residual >100mL
• Insulin 10U IV + D50 25g IV (90% response rate, K+ ↓ 0.6-1.2 mEq/L)
• Albuterol 10-20mg neb (60-80% respond, K+ ↓ 0.5-1.0 mEq/L)
• Synergistic effects when combined • Monitor glucose hourly × 6hrs
• If respiratory acidosis: Improve ventilation (each 0.1 pH ↑ = 0.6 mEq/L K+ ↓)
• Give ASAP, don't wait 1-2 hours • Onset: 1 hour, K+ ↓ 0.4 mEq/L @ 1hr, 0.7 mEq/L @ 4hrs • Works in small intestine
💊 LOKELMA: Give IMMEDIATELY, Don't Wait!
⏰ Timing is Critical
Common Mistake: Waiting 1-2 hours after insulin/albuterol to give Lokelma
Correct Approach: Give Lokelma IMMEDIATELY with other treatments
✅ Why Give ASAP:
- 1-hour onset means earlier benefit
- Synergistic with shifting agents
- Prevents K+ rebound after insulin wears off
- Provides sustained K+ removal
- May prevent need for dialysis
🚫 Lokelma Won't Work If:
- Bowel obstruction (works in small intestine)
- Severe gastroparesis
- Recent bowel surgery
- Inability to take PO medications
- Ileus or severe constipation
🧠 Mechanism: Small Intestine Action
Lokelma (sodium zirconium cyclosilicate) works primarily in the small intestine by exchanging sodium and hydrogen for potassium. This is why it won't work in bowel obstruction - the medication must reach the small intestine to be effective.
🔍 Comprehensive Etiology: Why Is K+ High?
📋 Systematic Approach to Hyperkalemia Causes
💀 Cellular Death/Lysis
Massive K+ Release from Cells
- Rhabdomyolysis: Muscle cell breakdown
• CPK >1000, myoglobin in urine • Check for dark/coca-cola urine - Tumor Lysis Syndrome: Oncology emergency
• Chemotherapy initiation • High LDH, uric acid, phosphate - Gut Ischemia: Intestinal cell death
• Mesenteric ischemia • Often with severe acidosis - Massive Hemolysis: RBC destruction
• Check LDH, haptoglobin, indirect bilirubin - Compartment Syndrome: Muscle necrosis
• Trauma, prolonged immobilization - Massive Burns: Tissue destruction
• >20% body surface area • Peak K+ at 24-48 hours - Malignant Hyperthermia: Anesthesia emergency
• Succinylcholine trigger • Hyperthermia + rigidity
🫘 Renal Causes
Impaired K+ Excretion
- RAASi Blockade: Most common cause
• ACE inhibitors, ARBs, spironolactone • Aldosterone receptor antagonists - Low Distal Sodium Delivery: Volume depletion
• Dehydration reduces distal Na+ delivery • Less K+ exchange in collecting duct - AKI/CKD: Reduced nephron mass
• eGFR <30: high risk • Oliguria/anuria - Type 4 RTA: Hypoaldosteronism
• Diabetes, NSAIDs, heparin • Normal anion gap acidosis - Calcineurin Inhibitors: Tacrolimus, cyclosporine
• Impairs distal K+ secretion - Trimethoprim/Pentamidine: ENaC blockade
• Blocks sodium channels in collecting duct - Gordon Syndrome: Pseudohypoaldosteronism type II
• Thiazide-sensitive hypertension + hyperkalemia
🏥 Endocrine Disorders
Hormonal Dysregulation
- Addison's Disease: Primary adrenal insufficiency
• Low cortisol AND aldosterone • Hyperpigmentation, hypotension - Congenital Adrenal Hyperplasia: 21-hydroxylase deficiency
• Salt-wasting crisis in newborns • Virilization - Hypoaldosteronism: Selective mineralocorticoid deficiency
• Diabetes, HIV, elderly • Normal cortisol - Hyporeninism: Low renin state
• Diabetic nephropathy • NSAIDs, β-blockers
🔬 Pseudohyperkalemia
Falsely Elevated Lab Values
- Hemolysis: Most common pseudo-cause
• Check hemolysis index • Repeat with careful draw - Thrombocytosis: Platelet clumping
• PLT >1,000,000 • Use heparinized tube - Extreme Leukocytosis: WBC breakdown
• WBC >100,000 • Leukemia, lymphoma - Fist Clenching: During phlebotomy
• Muscle contraction releases K+ - Difficult Draw: Prolonged tourniquet
• Cellular release from ischemia - Hereditary Spherocytosis: Fragile RBCs
• Family history, spherocytes on smear - Stored Blood: Transfusion-related
• Blood >7 days old • Massive transfusion protocol
📈 Increased K+ Intake
- Salt Substitutes: KCl instead of NaCl
• "NoSalt", "Morton Salt Substitute" - IV Potassium: Iatrogenic
• High-dose K+ replacement - High-K+ Foods: Usually not sole cause
• Bananas, oranges, potatoes in CKD - Blood Transfusions: Especially massive
• Each unit contains ~5-7 mEq K+ - Herbal Supplements: Noni juice, alfalfa
• Often overlooked in history
🔄 Transcellular Shifts
- Acidosis: K+ shifts out of cells
• Each 0.1 pH ↓ = ~0.6 mEq/L K+ ↑ - Insulin Deficiency: DKA
• Total body K+ often low despite high serum - β-blocker Overdose: Impaired cellular uptake
- Hypertonicity: Water shifts out
• Hyperglycemia, mannitol - Succinylcholine: Depolarizing paralytic
• Especially in burn/trauma patients - Digitalis Toxicity: Na-K-ATPase inhibition
• Check digoxin level • Avoid calcium if suspected - Intense Exercise: Muscle K+ release
• Heat stroke, dehydration • Usually transient
🧬 Genetic/Congenital
Hereditary Disorders
- Hyperkalemic Periodic Paralysis: Sodium channel mutations
• Episodes triggered by K+ intake, cold, rest after exercise - Pseudohypoaldosteronism Type I: Mineralocorticoid resistance
• Autosomal recessive • Salt wasting, failure to thrive - Pseudohypoaldosteronism Type II: Gordon syndrome
• Thiazide-sensitive hypertension + hyperkalemia - Sickle Cell Disease: Renal tubular dysfunction
• Type 4 RTA pattern • Chronic hemolysis
💊 Additional Medications
Often Overlooked Drug Causes
- Heparin (UFH/LMWH): Aldosterone suppression
• Usually after 4+ days • Check aldosterone level - NSAIDs: Multiple mechanisms
• Reduced renin, prostaglandin inhibition • Type 4 RTA - Immunosuppressants: Beyond calcineurin inhibitors
• Sirolimus, everolimus - α-agonists: Clonidine, methyldopa
• Central sympathetic suppression - Mannitol: Hyperosmolar-induced shift
• Especially in neuro ICU patients
🚨 Critical Care Causes
ICU-Specific Scenarios
- Massive Tissue Trauma: Crush injuries
• Earthquake victims • Prolonged entrapment - Reperfusion Injury: After ischemia
• Tourniquet release • Revascularization procedures - Ventilator-Associated: Respiratory acidosis
• Acute CO2 retention • Check ABG - Post-Cardiac Arrest: Cellular injury
• Global hypoxic-ischemic injury
🚨 HIGH-YIELD Clinical Correlations
Classic combo - dehydration ↓ distal Na+ delivery + ACE-I blocks aldosterone = severe hyperkalemia
Normal ECG + extreme K+ (>8) + no symptoms = likely false positive
Hyperkalemia + AKI + dark urine = check CPK, treat aggressively
Hyperkalemia + hyponatremia + hypotension + hyperpigmentation
Hyperkalemia + hypertension + normal GFR = think thiazide trial
Hyperkalemia + dig toxicity = NO CALCIUM (causes "stone heart")
📊 EKG Manifestations of Hyperkalemia
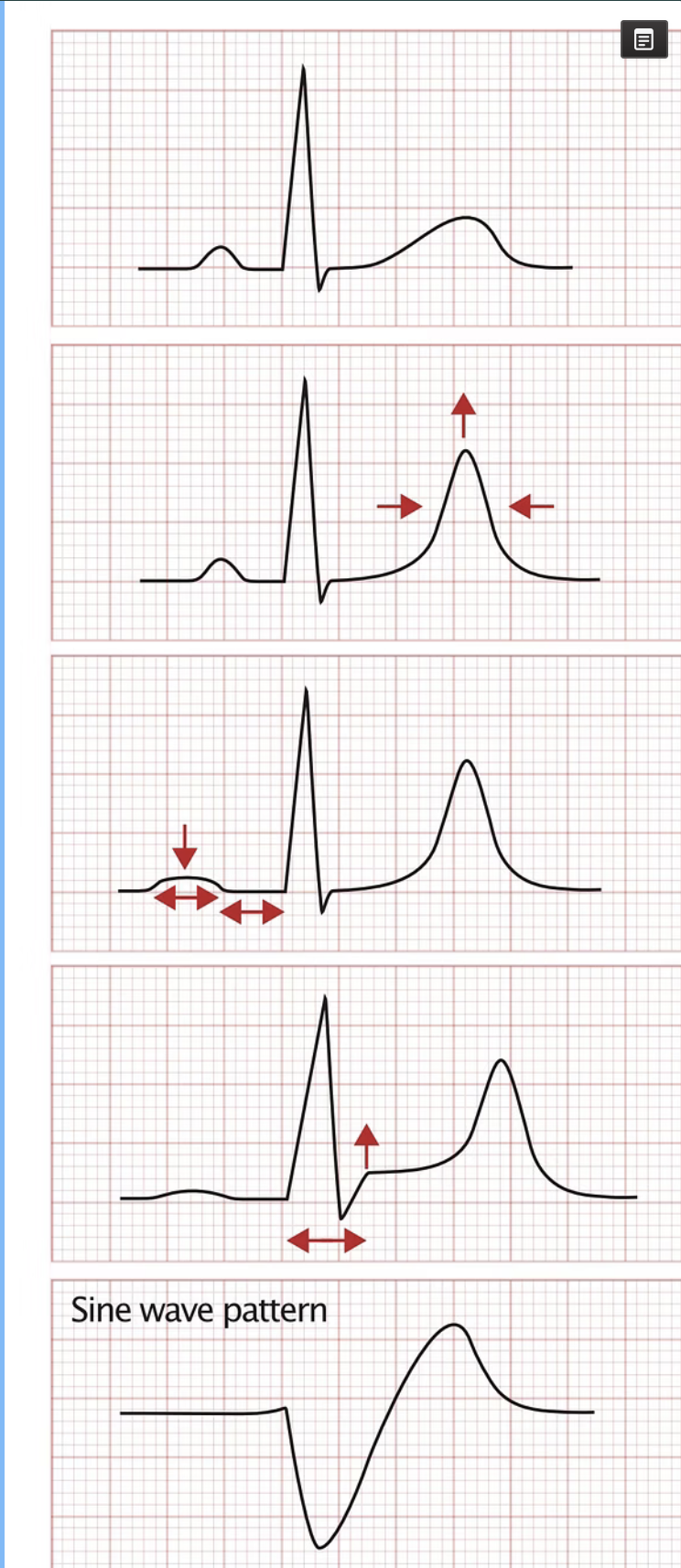
1. Mild Hyperkalemia
2. Moderate Hyperkalemia
3. Severe Hyperkalemia
4. Critical Hyperkalemia
🔍 Diagnostic Workup
📋 Essential Labs
- Repeat K+: Confirm result, rule out hemolysis
- BMP: Check BUN/Cr, bicarb, glucose
- Magnesium: Often overlooked contributor
- ABG: If acidosis suspected
- CPK: If rhabdomyolysis suspected
⚡ Immediate Assessment
- 12-Lead ECG: Look for peaked T waves
- Bladder Scan: Check for retention FIRST
- Cardiac Monitor: Continuous rhythm monitoring
- Vital Signs: Blood pressure, heart rate
- Muscle Strength: Weakness, paralysis
- Reflexes: Diminished or absent
🔍 Etiology Investigation
- Medication Review: ACE-I, ARB, K+ sparing diuretics
- Kidney Function: AKI, CKD assessment
- Endocrine: Adrenal insufficiency, hypoaldosteronism
- Tissue Breakdown: Rhabdomyolysis, tumor lysis
- GI Function: Bowel obstruction (affects Lokelma)
- Dietary History: Salt substitutes, supplements
💊 Treatment Mechanisms & Timing
🛡️ Membrane Stabilization
Calcium (No K+ Effect)
- Calcium Gluconate: 30mL IV (peripheral OK) - 9% elemental Ca
- Calcium Chloride: 10mL IV (central line only) - 27% elemental Ca
- ⚡ KEY: CaCl₂ has 3× MORE elemental calcium than gluconate
- Success Marker: QRS narrowing (not T wave flattening)
- Onset: 1-3 minutes
- Duration: 30-60 minutes
- Mechanism: Stabilizes cardiac membrane
- Caution: Avoid in digoxin toxicity
🔄 Potassium Shifting
Evidence-Based Intracellular Shifting
- Insulin + Glucose: MOST RELIABLE
• K+ ↓: 0.6-1.2 mEq/L • Onset: 15-30 min • Duration: 4-6 hrs • ~90% response rate
• Standard: 10U regular insulin IV + 25g dextrose (if glucose <250) - Albuterol: VARIABLE effectiveness
• K+ ↓: 0.5-1.0 mEq/L • Onset: 30-60 min • Duration: 2-4 hrs • Only 60-80% respond
• Dose: 10-20mg nebulized • Higher doses (20mg) more effective
• Less reliable in ESRD patients • Use as adjunct to insulin - Sodium Bicarbonate: CONTROVERSIAL - Limited evidence
• Only effective if severe metabolic acidosis (pH <7.1-7.2)
• Minimal effect in normal pH • May cause volume overload, alkalosis
• Dose: 50-100 mEq IV if pH <7.1 • Avoid in mild acidosis - Respiratory Acidosis Treatment: Address underlying cause
• Mechanical ventilation: ↑ minute ventilation, ↓ PCO₂
• Each 0.1 pH ↑ = ~0.6 mEq/L K+ ↓ • Treat airway obstruction, respiratory depression
• BiPAP/CPAP for acute respiratory failure • Bronchodilators if indicated
🎯 Clinical Evidence & Recommendations:
• Insulin + glucose combo
• Most predictable response
• Works in all patient populations
• Albuterol as adjunct
• Bicarbonate only if pH <7.1
• Treat respiratory acidosis
🗑️ Potassium Removal
Eliminates K+ from Body
- Lokelma: 10g PO IMMEDIATELY (don't wait!)
- Patiromer: Once daily dosing
- Hemodialysis: Most effective for severe cases
- Lokelma onset: 1 hour (small intestine)
- Dialysis: 1 mEq/L in 60 min
- Note: Foley catheter first if no EKG changes
🆚 Potassium Binder Comparison: New Generation vs Traditional
| Parameter | Lokelma (SZC) | Veltassa (Patiromer) | Kayexalate (SPS) |
|---|---|---|---|
| FDA Approval | 2018 | 2015 | 1950s |
| Exchange Ion | Sodium + Hydrogen | Calcium | Sodium |
| Site of Action | Small intestine | Colon | Colon |
| Onset of Action | 1 hour (0.4 mEq/L) | ~7 hours | ~2 hours |
| Dosing Frequency | TID loading, then daily | Once daily | Every 6-8 hours |
| Bowel Obstruction | Won't work | May still work (colon) | May still work (colon) |
| Major Side Effects | Edema, fluid retention | Hypomagnesemia | Colonic necrosis risk |
| Clinical Use | Acute & chronic (give ASAP) | Chronic management | Acute (use with caution) |
⚖️ Dialysis vs Conservative Management Decision
The choice between aggressive intervention (dialysis) and conservative management depends critically on EKG changes and ability to establish urine output:
🚰 Conservative Management
When appropriate:
- No EKG changes
- K+ 5.5-7.0 mEq/L
- Able to establish UOP
- No severe symptoms
Start with: Foley catheter
🏥 Aggressive Management
When needed:
- ANY EKG changes
- K+ >7.5 mEq/L
- Anuric/oliguric
- Severe symptoms
Prepare for: Emergent dialysis
🚰 Urinary Obstruction: The Great Mimicker
Often overlooked but rapidly reversible cause that can prevent the need for dialysis
⚠️ Common Pitfalls & Evidence-Based Corrections
🚫 Avoid These Mistakes
- Central line first: Place Foley BEFORE central line if no EKG changes
- Delaying Lokelma: Give IMMEDIATELY, don't wait 1-2 hours
- Bicarbonate routine use: Only effective if pH <7.1-7.2
- Expecting albuterol to work: Only 60-80% respond (vs 90% for insulin)
- Missing respiratory acidosis: Treat underlying ventilation issues
- Calcium in Digitalis Toxicity: Can precipitate "stone heart"
- Insulin without Dextrose: Risk of severe hypoglycemia
👀 Monitor Closely
- Urine Output: After Foley placement
- QRS Width: Calcium success = QRS narrowing (not T waves)
- Glucose: Hourly × 6h after insulin (90% respond)
- Albuterol Response: Only 60-80% will respond
- Respiratory Status: If acidosis present, treat underlying cause
- Potassium: Every 2-4 hours initially
- ECG: Continuous monitoring if changes present
✅ Evidence-Based Success
- Insulin + Glucose: Most reliable shifting agent (Grade A evidence)
- QRS Narrowing: Primary indicator of calcium effectiveness
- K+ Reduction >0.5 mEq/L: Within 1 hour of treatment
- Bicarbonate Response: Only if severe acidosis (pH <7.1)
- Respiratory Improvement: Each 0.1 pH ↑ = 0.6 mEq/L K+ ↓
- Urine Output >0.5 mL/kg/hr: After Foley placement
- Avoided Dialysis: Conservative management successful
🧮 Enhanced Hyperkalemia Calculator
Comprehensive Treatment Protocol Calculator
🎯 Enhanced Key Learning Points
🚰 Foley First Principle
- First catheter = Foley (not central line)
- If no EKG changes, establish UOP first
- May prevent need for dialysis
- Check bladder scan in all cases
💊 Lokelma Timing
- Give IMMEDIATELY, don't wait
- Works in small intestine
- Won't work in bowel obstruction
- 1-hour onset for K+ reduction
⚡ Emergency Priorities
- EKG changes = immediate calcium
- CaCl₂ has 3× MORE elemental Ca than gluconate
- QRS narrowing = calcium success (not T waves)
- Stabilize → Foley → Shift → Remove
- Continuous cardiac monitoring
- Don't wait for labs to treat severe cases
🔍 Etiology Recognition
- Cellular death: Rhabdo, tumor lysis, gut ischemia
- Renal: RAASi blockade, volume depletion, CKD
- Endocrine: Addison's disease, CAH
- Pseudohyperkalemia: Hemolysis, thrombocytosis
- Genetic: Hyperkalemic periodic paralysis
- Critical care: Burns, reperfusion injury