📚 Related Urinalysis Modules
🔬 Interpretation Fundamentals
Core principles and systematic approach
🔬 Ancillary Urine Testing
Microscopy, FeNa analysis, and urine eosinophil testing
🦠 UTI Assessment
UTI detection, pitfalls, and evidence-based evaluation
⚠️ DIPSTICK LIMITATIONS: When Chemistry Lies
🎭 The Great Deception
Dipsticks were designed for screening, not diagnosis. Relying solely on dipstick results in nephrology is like diagnosing MI with only a cholesterol level.
🔴 False Positive Protein
- Concentrated urine (dehydration)
- Alkaline urine (pH >8)
- Gross hematuria
- Quaternary ammonium compounds
- Phenazopyridine (Pyridium)
❌ False Negative Protein
- Dilute urine (overhydration)
- Non-albumin proteins (light chains)
- Very acidic urine
- Early diabetic nephropathy
- Microalbuminuria levels
🩸 Blood Detection Issues
- Detects hemoglobin, not RBCs
- Free hemoglobin from hemolysis
- Myoglobin from rhabdomyolysis
- Misses intact RBC in dilute urine
- Oxidizing agents cause false positives
🦠 Leukocyte Esterase Limits
- Doesn't detect all bacteria
- False positive in vaginal contamination
- Doesn't differentiate infection from inflammation
- Poor sensitivity in early UTI
- Trichomonas can cause false positives
🎯 Clinical Bottom Line
"Treat the patient and the microscopy, not the dipstick." - A negative dipstick with an active urinary sediment should prompt immediate investigation, not reassurance.
🧪 Complete Urinalysis Dipstick Analysis
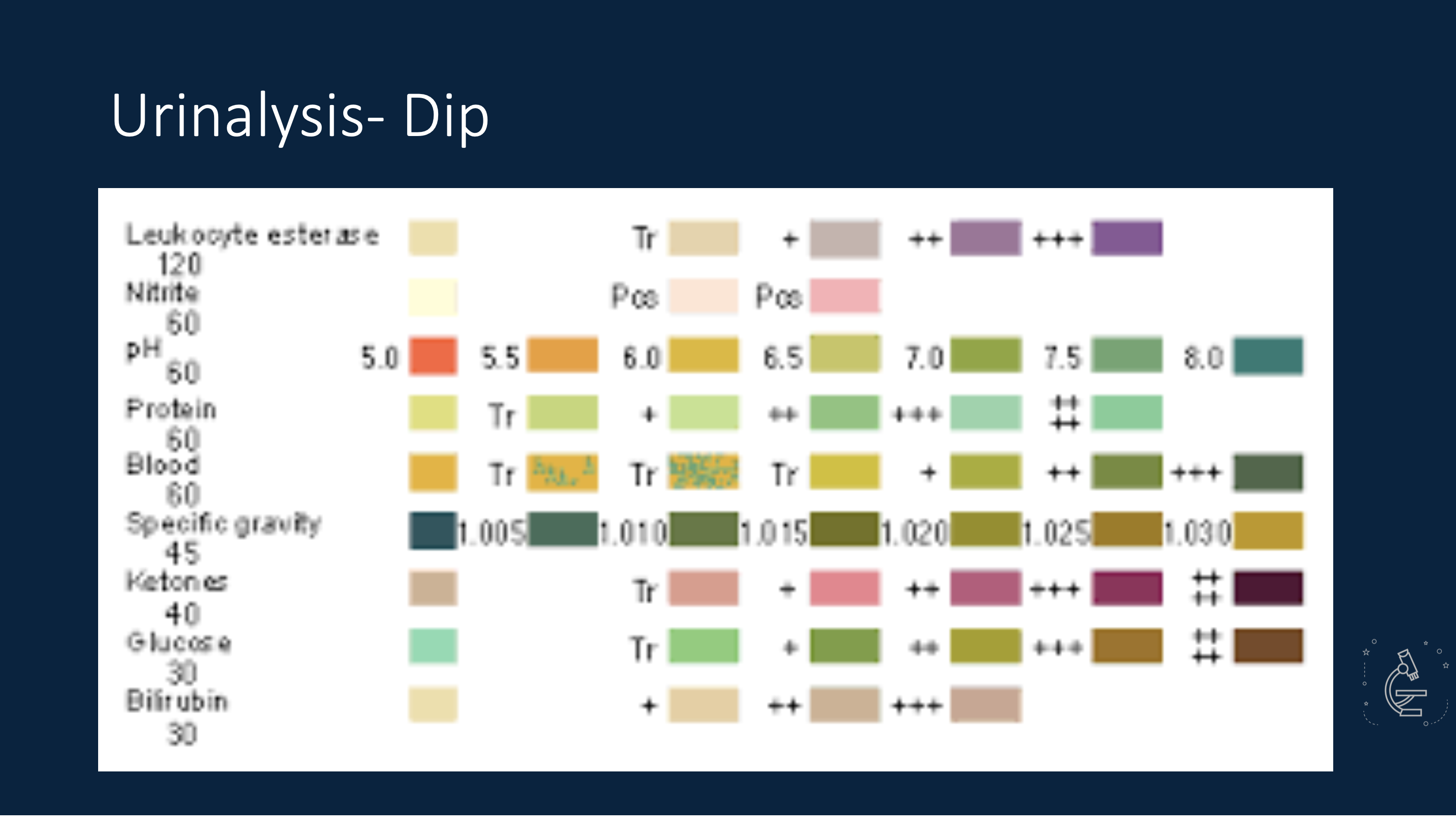
Dipstick: The Screening Tool Reality Check
Remember: Dipsticks are designed for screening, not diagnosis. Each parameter has specific limitations and timing requirements that affect accuracy.
⚠️ False Positives
Concentrated urine, medications, contaminants can create misleading results requiring clinical correlation.
❌ False Negatives
Dilute urine, timing issues, and specific protein types can be missed by standard dipstick testing.
⏰ Timing Critical
Many parameters require specific collection timing and proper specimen handling for accuracy.
🧪 Dipstick Parameter Deep Dive
🟦 Specific Gravity (1.005-1.030)
Hydration Status Indicator
- Low (<1.010): Overhydration, diabetes insipidus, diuretics
- High (>1.025): Dehydration, SIADH, contrast agents
- Fixed (1.010): Chronic kidney disease
- Clinical Pearl: Reflects concentrating ability
🍋 pH (4.5-8.0)
Acid-Base and Stone Risk
- Acidic (<6.0): Metabolic acidosis, high-protein diet, cranberry juice
- Alkaline (>7.5): UTI with urease-producing bacteria, vegetarian diet
- Stone Risk: Uric acid (acidic), calcium phosphate (alkaline)
- False Alkaline: Old specimens, bacterial overgrowth
🟡 Protein (negative to trace)
Glomerular Function Screen
- Detects: Primarily albumin (not light chains, low molecular weight proteins)
- False Positive: Concentrated urine, alkaline pH >8, gross hematuria
- False Negative: Dilute urine, non-albumin proteins (Bence Jones)
- Follow-up: Spot urine albumin/creatinine ratio for quantification
🍭 Glucose (negative)
Diabetes and Tubular Function
- Threshold: ~180 mg/dL serum glucose (renal threshold)
- Positive: Diabetes, stress hyperglycemia, pregnancy
- Renal Glucosuria: Normal serum glucose, tubular defect
- False Negative: Ascorbic acid, old specimens
🟢 Ketones (negative)
Metabolic Status Indicator
- Diabetic Ketoacidosis: Life-threatening emergency
- Starvation: Prolonged fasting, low-carb diets
- Other Causes: Alcoholism, pregnancy, hyperthyroidism
- Limitation: Detects acetoacetate, NOT β-hydroxybutyrate
🔴 Blood/Hemoglobin (negative)
Hematuria vs Hemoglobinuria
- Detects: Hemoglobin peroxidase activity (RBCs, free Hgb, myoglobin)
- True Hematuria: Requires microscopy to see intact RBCs
- Hemoglobinuria: Intravascular hemolysis, no RBCs on micro
- Myoglobinuria: Rhabdomyolysis, no RBCs on micro
🦠 UTI Detection: Timing is Everything
🟠 Leukocyte Esterase
What it detects: Enzyme from neutrophils (indirect measure of pyuria)
- Timing: No specific bladder dwell time required
- Sensitivity: 48-71% (varies by pathogen)
- Lower with: Enterococcus, Klebsiella infections
- False Positive: Trichomonas, vaginal contamination
- False Negative: Antibiotics, high glucose/protein
🟡 Nitrites - The 4-Hour Rule
Critical Timing: Bacteria need ≥4 hours in bladder to convert nitrates to nitrites
- High Specificity: 95% (positive = likely UTI)
- Poor Sensitivity: 23-38% (negative doesn't rule out UTI)
- False Negative: Frequent urination, non-nitrate reducers
- Organisms: E. coli, Klebsiella, Proteus (positive)
- Won't Detect: Enterococcus, Staph, Pseudomonas
⏰ Why Timing Matters for Nitrites
✅ Optimal Conditions
First morning void: Urine in bladder overnight (≥4 hours) allows bacterial enzyme activity to convert dietary nitrates to detectable nitrites.
❌ False Negative Scenarios
Frequent urination: Infants, elderly, overhydration, diuretics - insufficient dwell time for nitrate conversion.
🦠 Bacterial Specificity
Enterobacteriaceae only: Gram-negative organisms have nitrate reductase. Many Gram-positive bacteria lack this enzyme.
🎯 Clinical Integration
Best Approach: Combine LE + Nitrites + clinical symptoms. Sensitivity improves to 94% when both tests used together.
⚖️ Dipstick vs Microscopy: Head-to-Head Comparison
🥊 The Ultimate Diagnostic Showdown
📊 Dipstick Testing
The Screening Tool
- Rapid results (1-2 minutes)
- No microscope required
- Standardized chemistry
- Cost-effective screening
- Point-of-care capability
- High false positive/negative rates
- Cannot assess cell morphology
- Misses casts entirely
- No contamination assessment
- pH and concentration dependent
🔬 Microscopy
The Diagnostic Gold Standard
- Direct visualization of pathology
- RBC morphology assessment
- Cast identification and typing
- Contamination evaluation
- Crystal characterization
- Infection vs inflammation
- Requires trained personnel
- Time-consuming (10-15 minutes)
- Operator dependent
- Fresh specimen needed
- Equipment requirements
🎯 When Each Method Excels
📊 Dipstick Best For:
- Initial screening in asymptomatic patients
- Point-of-care testing in clinics
- Monitoring known conditions (diabetes, proteinuria)
- Large-scale population screening
- Resource-limited settings
🔬 Microscopy Essential For:
- AKI evaluation and management
- Hematuria workup and differentiation
- Glomerular disease detection
- UTI confirmation vs contamination
- Stone disease evaluation
- Any nephrology consultation
🧠 The Nephrology Perspective
🎯 Perfect Scenario
Use dipstick for rapid screening, ALWAYS follow with microscopy when abnormal or when clinical suspicion exists.
⚠️ Never Do This
Don't diagnose or rule out kidney disease based on dipstick alone. Don't ignore active sediment because dipstick is normal.
📝 Clinical Reality
In practice, combine both methods with clinical context for optimal diagnostic accuracy and patient care.
🧪 Additional Dipstick Parameters
🟨 Bilirubin (negative)
Liver Function Indicator
- Conjugated bilirubin only: Water-soluble, filtered by kidneys
- Positive: Hepatitis, biliary obstruction, cirrhosis
- Early indicator: May appear before clinical jaundice
- False Positive: Phenazopyridine, rifampin
🟣 Urobilinogen (small amount normal)
Hepatic Function and Hemolysis
- Normal: 0.2-1.0 mg/dL (small amount from bacterial reduction)
- Increased: Hemolysis, liver disease, portal shunting
- Decreased/Absent: Biliary obstruction, antibiotics
- Best specimen: Afternoon urine (peak excretion)
🎯 Dipstick Mastery Summary
🧪 Screening Tool
- Designed for screening, not diagnosis
- Multiple false positive/negative scenarios
- Requires clinical correlation always
- Never replaces microscopy in nephrology
⏰ Timing Critical
- Nitrites require ≥4 hours bladder dwell
- Fresh specimens prevent bacterial overgrowth
- Collection method affects accuracy
- First morning void optimal for several parameters
🎯 Clinical Integration
- Combine with symptoms and microscopy
- Understand parameter-specific limitations
- Recognize interference patterns
- Use as supportive, not definitive data